Need Assistance? Call us today! 602-478-9713
I had barely walked in the door and introduced myself when Bob, a very bright engineer, started to talk.
“I know you’re not supposed to be able to help me,” he blurted, “because everything I read says that oral appliances shouldn’t work for me, but you’re the only chance I have. And I don’t believe everything I read anyway. Do you?”
Bob was obviously nervous. He spoke rapidly without taking a breath. I knew he had just spoken several sentences, but I never heard a period.
Interviewing is an art. To obtain the valuable information you need to help, some patients simply need to be coaxed, cajoled into sharing information that has heretofore fallen on deaf ears. To make the interview meaningful and useful, others require directed guidance to trust that this time it would be different. Neither was the case with Bob. Bob left no opportunity for me to answer his obviously rhetorical question, and without a breath, continued to talk. I quietly sat down to listen; knowing that my transcriptionist would not miss a word as she busily took notes.
Bob’s Initial Interview: The Art of Listening
Bob had a very severe condition of atrial fibrillation. Initially, the incidents were mild and could be controlled with medication. On several occasions, when there was real potential for a blood clot and a sub sequential stroke, he was rushed to the emergency room and treated with heparin and coumadin. His condition worsened and had progressed to the point where preventative medication had reached its dosage limits. In spite of the high level of preventative medication, he was having more and more severe episodes. He told of times when he was on very important business trips and an episode of atrial fibrillation would confine him to a hotel bed for forty-eight hours. His heart would beat over two hundred times a minute for twenty four hours, and it would take him another twenty four hours to recover. “It was exhausting, and very detrimental to my career,” he stated, his voice riddled with frustration.
Bob paused. And looked at me. There was a moment, maybe longer, of silence. He smiled, and continued. I almost had the feeling that he had read “How Doctors Think” by Dr. Jerome Groopman. Dr. Groopman queries, “The doctor is in, but is he listening?” He then describes the initial interview in which a patient is asked the first question, and reports that his research has revealed that the average time a patient is allowed to speak before being interrupted is eighteen seconds[1]. I found no reason to interrupt Bob; he was doing great.
Bob is an engineer for and a consultant to Air Products. He is involved in process safety, engineering principles that apply to industrial accidents. Not slips, trips and falls, but major explosions and chemical accidents. Following the World Trade Center attack, Bob helped develop thermobarric weapons that would kill the Taliban in their caves without destroying potential evidence. Such a career demands complete concentration and accuracy.
But Bob’s career was at risk. In addition to his own problems related to the atrial fibrillation, his wife suffered from a chronic pain condition which required him to assist her. The joint pressures of his personal and professional lives demanded that he pursue a solution to his episodes of atrial fibrillation. Bob was given a few options; the one that was recommended was an ablation procedure. Ablation is a procedure in which the source of a patient's heart arrhythmia is mapped, localized, and then ablated. Generally, ablation is accomplished by applying radiofrequency (RF) energy, applying electrical energy, or freezing the offending area through a catheter. This creates a small scar that is electrically inactive and thus incapable of generating heart arrhythmias. Many forms of cardiac arrhythmias have been rendered curable by ablation techniques over the past 15 years, but atrial fibrillation has remained a challenge. While the procedure is essentially safe, it is of course not without risk. Cardiac bleeding, the need for pacemaker placement, and a slight risk of death are among the list of concerns.[2]
The ablation procedure had been scheduled and Bob had been informed of the risks that included stroke and death. He was aware that this lengthy procedure, while potentially dangerous, had a strong possibility of correcting his atrial fibrillation. While waiting for the ablation appointment, Bob had serious a-fib episode and found himself in the hospital emergency room being evaluated by another cardiologist. It was this cardiologist who asked Bob if he ever had a sleep study, referring to the recent New England of Medicine Journal of Medicine articles associating sleep apnea with myocardial infarctions, stroke, diabetes, and atrial fibrillation.[3][4]
Although Lehigh Valley Hospital’s sixteen bed sleep lab didn’t have an opening for three months, Bob’s ablation procedure was coming up. Bob was moved up on the waiting list and was soon scheduled for his overnight polysomnogram.
The Polysomnogram
“Did you ever have a sleep test?” he asked me. I had spent several nights in a sleep lab observing PSG’s and had been tested at home with ambulatory studies, but no, I had never actually undergone an actual polysomnogram. He smiled as he lifted his eyebrows. “You oughta try it sometime,” he said with a sly grin.
I put my hand up to stop him. We were now going to talk about his diagnosis, and I had the polysomnomgram results in front of me. I noted that it was a “split night polysomnogram,” which means that halfway or so into the night the technicians had determined that the sleep disordered breathing was severe enough to proceed with a CPAP trial and titration. The diagnostic portion lasted four hours, and Bob’s sleep efficiency was only 38%. Sometimes that can be attributed to the “first night affect,”[5] but in Bob’s case it was most likely largely due to his severe obstructive disorder. Bob’s sleep was extremely fragmented, and despite the fact that he did not have severe drops in his oxygen levels and very few true “apneas,” Bob had a series of hypopneas (drops in oxygen levels of 3% or more) that prevented him from ever entering slow wave (restorative) sleep or rapid eye movement (REM) sleep. These episodes occurred more than once a minute. Loud snoring was noted as well. Bob’s hypopnea index (hypopneas per hour) was 72 and his apnea index (apneas per hour) was 4, giving him an apnea hypopnea index (AHI) of 76. In addition, there was a high degree of periodic leg movements (PLM’s). Bob was diagnosed with severe obstructive sleep apnea with associated snoring, sleep fragmentation and periodic leg movements.
“Hey, Doc, I bet YOU never wore a CPAP!”
All Bob wanted to talk about next was the CPAP. “You never wore one of THOSE, I bet.” Actually I had. While admitting that I personally didn’t find it very comfortable and couldn’t imagine trying to go to sleep with the mask in place, I noted that I did have many patients who just loved it and considered it their “life line.” “Well, good for them,” he smirked. “It was like trying to go to bed with your head out the car window traveling 90 miles an hour. But I tried. Boy, did I try.”
At the sleep lab, Bob kept the CPAP on for just under two hours, and with only 8 cm of water pressure Bob’s hypopneas stopped and he actually entered slow wave sleep. He was not asleep long enough to get into REM sleep, but it seemed clear that continuous positive airway pressure could be an answer for Bob--and the 8 cm of water really wasn’t that much pressure! These two positive indicators might have convinced Bob to tolerate the treatment.
Bob was given a CPAP unit, but noted when he tried to use it, he would have large amounts of fluid on his face and his pillow. Bob immediately returned to Will’s Eye Hospital where previously he had lacrimal duct surgery. It was explained that the check valve was not functioning in his lacrimal duct and that, as a result, he had essentially a direct connection from his nasal cavity to his eye. His surgeon made it very clear that CPAP was not an option for him.
Bob returned to his sleep doc who “had a contemptuous attitude for anything other than the CPAP or related devices, and seemed to actually have a contemptuous attitude towards me! He acted as though I wasn’t willing to try the CPAP, but with my eye…... the fluids….
To make it more graphic, when I blow my nose, I spatter the inside of my glasses! I just couldn’t do it. And he didn’t offer the oral appliance as an option.” Without commenting, I checked the chart and saw that Bob listed Vince, a friend of his, as his referral source to our office.
Vince’s Story
I remembered Vince. He was also an Air Products engineer. Vince was a tall, thin, young father of three who noted that he was having trouble staying focused at work. His snoring and witnessed apneas by his wife led to a sleep study, and he too eventually learned that he was CPAP intolerant. I remember how surprised he was that he had severe apnea. “Hey; I’m not heavy; I’m young; I’m healthy and active – certainly not the prototype of your typical apnea patient.” Vince hated the clinical feeling of using a CPAP in his own home. I remember him telling me he felt like he was in the hospital in his own bed! Vince’s dentist made him a Silent Night appliance, and while it helped his snoring, he kept breaking it. So Vince arrived at our office in search of a more “appropriate” appliance. After reviewing his polysomnomgram, we explained that while the oral appliance could be effective, we really wanted to be sure that he knew that the CPAP was the treatment of choice with severe apnea. “No way…been there; done that.” So, we gave him an oral appliance. When he went for a follow up polysomnogram with his new oral appliance, it revealed that his RDI of 58 was reduced to 2. His excessive daytime sleepiness condition resolved.
Clearly, Vince had talked to Bob. “I’ve done the research,” said Bob. “ I know that it is generally accepted that the oral appliance isn’t the first choice for severe apnea. But you can’t tell me that it can’t help severe cases. So can we give it a try? As I said, you’re my last hope.”
Is Bob a candidate for Oral Appliance Therapy?
Finally, it was my turn. I didn’t need to tell Bob much about his condition and how the oral appliance may help him, but I did need to explain some very important information about oral appliance therapy. Bob already knew there was no “guarantee.” He also knew that there were very few predictors in terms of oral appliance success. We needed now to determine if Bob was a candidate for oral appliance therapy, and then be sure that Bob knew about the potential side effects of the therapy.
Our initial oral exam quickly revealed that Bob could be fitted for an oral appliance. Among the requirements is a sufficiently healthy dentition to act as an anchor for both arches, as well as a sufficient range of motion that would allow us to maintain the mandible forward during the night when the musculature tone drops tending to allow the tongue and the mandible to fall back. His hopeful response to this information decreased only slightly when I told him, “But there is more.”
Bob’s engineering instincts became obvious; he needed to know how this proposed appliance worked. And I didn’t hesitate to give him the explanation.
The CPAP works by creating an internal splint of the airway that tends to collapse when we sleep because of a decrease in the muscle tone that is responsible to keep the airway open. The oral appliance works by creating some degree of muscular tension on the pharyngeal muscles, and thus creates a muscular external splint keeping the airway open. Keeping the jaw forward at night also tends to put tension on the tensor veli pallatini, creating tension in the soft palate, and also tends to counteract the relaxation of the genioglossus muscle, keeping the tongue from sealing against the soft palate. [6]
“But just like any therapy, there are some potential complications,” I said. “Just as when we use crutches to support a sprained ankle and we ask our biceps and triceps to work harder to provide that support, when we use an oral appliance, we ask our jaw muscles and our joints to be compromised during the night to support the airway. Consequently, just as we would want to be certain that your arms were healthy before we gave you crutches; we need to do some studies on your jaw muscles and temporomandibular joints before we consider an oral appliance. “
The examination continued. We used joint vibration analysis from BioRESEARCH to determine that his joints were indeed functioning within normal limits without internal derangements or degenerative joint disease.[Figure 1] In addition, computerized jaw tracking recorded his range of motion, and our clinical examination revealed no contraindication to oral appliance therapy [Figure 2]. The potential side effects of joint strain, muscle strain, and possible occlusal changes were reviewed. It was clear that Bob was eager to begin therapy, and that it was now in our hands to manage any dental or craniomandibular complication, as certainly there was much to be gained by successful therapy. After all relevant data was reviewed; together we decided to proceed with therapy. Impressions were made and a bite registration using a George Gauge was taken [Figure 3].
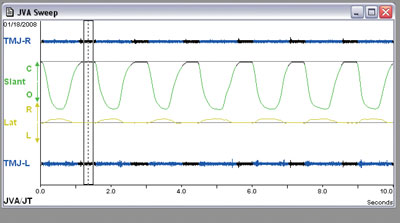
Figure 1. A joint vibration analysis of a patient without vibration episodes and joints functioning within normal limits.
Figure 2. This readout shows the results of a computerized jaw tracking, demonstrating a normal range of motion with the potential protrusion of 9.6 mm.
Figure 3a, 3b, 3c. The George Gauge (Great Lakes Ortho) is a valuable instrument for taking a proper bite registration for oral appliance therapy. 3a. The George Gauge is being used to help determine and record the initial degree of protrusion the dental appliance will provide. 3b. That degree of protrusion and the maxilla/mandibular relationship can be easily recorded with quick setting bite registration paste on a removable bite fork. 3c. The gauge will help determine the amount of potential protrusion, as well as the mark the amount of protrusion chosen for the initial anterior positioning of the mandible.
The Appliance Insertion and Bob’s Response
Three weeks later Bob’s appliance was inserted [Figures 4,5 and 6]. Titration and home care instructions were given, and a follow up appointment in three weeks was arranged. Bob showed up for his three week appointment – without his appliance. After seating Bob, Traci, our assistant, asked to see the appliance; he told her that he didn’t bring it. “Now how can we adjust it if you didn’t bring it?” she asked. “That’s why I didn’t bring it,” he responded. “I won’t let ANYBODY touch it.!” This protective response was indeed a good sign.
![Figure 4. This appliance (SomoDENT [SomnoMED]) is an excellent example of the type of a titratable, durable, mandibular advancement splint that can be used in the treatment of diagnosed sleep apnea when indicated.](https://asba.net/wp-content/uploads/2021/05/fig-4.jpg)
Figure 4. This appliance (SomoDENT [SomnoMED]) is an excellent example of the type of a titratable, durable, mandibular advancement splint that can be used in the treatment of diagnosed sleep apnea when indicated.

Figure 6. The Thorton Adjustable Positioner (TAP), is another excellent appliance used in Dental Sleep Medicine. This is an example of the TAP III.
Bob had responded quickly to appliance therapy. He reported that he stopped snoring and that his wife reported he had stopped kicking his legs. He was now waking up feeling refreshed, and aware that he was for the first time getting a full night’s sleep. What was even more amazing is that Bob had no bouts of atrial fibrillation - the first time in recent history that he went this long without some evidence of an a-fib event. Bob had no difficulty getting used to the appliance, in fact he had far less difficulty than most, and showed no signs of joint or muscle pain.
Bob was referred back to his sleep physician, but as one could have predicted, he refused to go. He was quite upset at the way he had originally been treated, and even more upset that the oral appliance was never discussed. A referral was made to another sleep doctor, a doctor in our sleep network who was very familiar with oral appliance therapy. Dr. Schellenberg reviewed the record and was thrilled that Bob had responded so well to oral appliance therapy. He felt that at this time a follow up PSG was not indicated. By this point Bob had gone several months without a bout of atrial fibrillation.
One full year had passed. Bob had one recall visit. The appliance was checked and continued to be functional. Bob had no dental changes and no joint or muscle pain or dysfunction. Bob had been scheduled for a recall visit, but before that appointment we received an “emergency phone call” from the Lehigh Valley Hospital. Bob had been admitted as an inpatient via the ER with a serious atrial fibrillation event. Bob’s appliance had broken the day before, and he planned to call the office the next day. The very first night he spent without the appliance resulted in a bout of atrial fibrillation.
Recently Bob had a follow up polysomnogram. Interestingly, Bob still has an AHI above normal, but significantly less than the original AHI of 76. As a result, we are currently titrating the appliance and will be monitoring the success of the titration with ambulatory studies. Bob continues to do well and has had no further a-fib events. He rejoices that his quality of life has improved dramatically.
The Challenges that Face Dentistry
While Bob’s story isn’t a common one – not everyone responds as positively to oral appliance therapy so quickly – there are many points to be gleaned from the experience.
First and foremost, dentistry has the potential to provide a very useful solution for patients with obstructive disorders.[7][8][9] However, in order to be able to provide that service, the practice model that we have become comfortable with in dentistry must be examined and altered. We must learn to work and communicate with our medical colleagues in a meaningful way. We must understand that our therapy will have degrees of success and not be as predictable as we have learned our general dentistry can be. We must learn interviewing techniques that may have not been required in our general dental settings; and we must learn how to educate and motivate not only the public, but also our physicians who in many cases, as in this case, may have a bias against dental therapy. Unfortunately, dental sleep medicine has the potential to create a competitive environment with our medical colleagues, and unless we change that environment, the patient will not be given the therapy that may be in their best interest.
We know that patients with obstructive disorders have significant potential to develop the co-morbities of stroke, myocardial infarctions, heart attacks, gastroesophageal reflux disease (GERD), and diabetes. There is also a serious concern for the associated snoring and excessive daytime sleepiness that can lead to depression, marital conflicts, motor vehicle and work related accidents.
Over ninety percent of the disorder remains undiagnosed [10.] Dentistry, in this author’s opinion, should be the number one portal of patients into sleep medicine. Very basic questions can lead to the suggestion of the potential of the disorder and a proper referral [Figure 7]. It is extremely important that dentists understand that obstructive disorders are a continuum that starts with snoring at one end and has severe apnea on the other, and that snoring should never be treated without proper diagnosis [Figure 8].
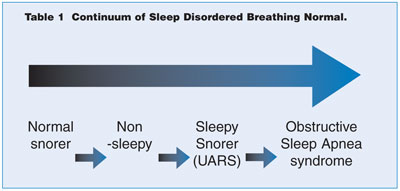
Figure 7. Sleep disturbed breathing in the form of obstructive disorders are a continuum. It is essential that snoring not be treated until a complete diagnosis is made.
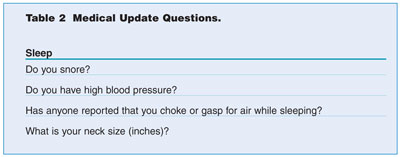
Figure 8. These questions should be asked during patients’ medical update at their dental recall visit. Positive responses are predictive for obstructive sleep disorders.
The following is the current policy statement from the American Academy of Sleep Medicine:
Oral Appliances are indicated in patients with mild to moderate OSA who prefer their use to continuous positive airway pressure (CPAP) treatment or who are inappropriate candidates for or who are refractory to CPAP treatment.[11]
It should be noted that this statement does NOT suggest that Oral Appliance Therapy (OAT) SHOULD be the first line of therapy in all cases. Nor does it suggest that it OAT is inappropriate for severe cases. Bob’s case is a perfect example of this concept.
A look at the history of dentistry reveals that our profession has faced challenges in the past. Our profession is facing its greatest challenge, the challenge to truly step out of the box of dentistry and become physicians of the oral cavity. We have learned that our skills can be helpful, and at times required, in the diagnosis and treatment of our patient’s chronic pain, joint dysfunction, headache, and recently even migraine, a true trigeminally mediated disorder (TMD). And now we need to add obstructive sleep disorders to that list. We have learned that bruxism is a parasomnia of sleep and that it too can be related to arousals and alterations in sleep architecture, as well as affecting the ability of the trigeminal nucleus to modulate nociceptive afferent activity. In addition, we have learned that some of the first signs of GERD , which is possibly associated with obstructive disorders, can have dental signs as their first indication of the disorder.
Sleep, then, becomes very important to the dentist. It is during sleep that the obstructive disorders exist. It is during sleep that our patients tend to parafunction, creating the forces that threaten our patients and our everyday dentistry. We are faced with the challenge to understand sleep and our role in diagnosing and treating patients with obstructive disorders and the parasomnia of bruxism. Accepting this challenge will indeed improve the lives of our patients.
References