Need Assistance? Call us today! 602-478-9713
By Dr. Felix Liao, DDS, MAGD, ABGD, D’ASBA
"You see only what you know, hence you can’t diagnose what you don’t know."
-Dr. Richard Beistle, DDS-
Obstructive Sleep Apnea “OSA” affects 1/7 of adults ages 30-69 worldwide1. The US ranks 2nd behind China in OSA prevalence with AHI > 5, and 4th with AHI >15 behind China, India, and Brazil. “Untreated OSA is associated with significant comorbidities and mortality. These represent a tremendous threat to the individual and global health.”1
As such, OSA impacts dental patients and their dentists, and medical patients and their doctors., and their families and staff. What’s behind OSA besides diabetes, obesity, and aging? Why wait until patients (or you the doctor), need rescuing with a CPAP or ventilator?
“A healthy mouth is more than healthy teeth”, states US Surgeon General David Satcher, MD, in Oral Health America 2000 2. In 2017, ADA adopted the following policy: “Dentists are encouraged to screen patients for sleep-related breathing disorders (SRBD) as part of comprehensive medical and dental history to recognize symptoms such as daytime sleepiness, choking, snoring or witnessed apneas and an evaluation for risk factors such as obesity, retrognathia, or hypertension.”3
This means “dentists can and should play an essential role in the multidisciplinary care of patients with certain SRBD and are well positioned to identify patients at increased risk”, states Dr. Jeffrey Cole, President of ADA.4
In said context, this article presents three new concepts that can restore 70-90% of patient’s oral-systemic complaints.
• Impaired Mouth Syndrome: a vast set of medical, dental, and mood symptoms stemming from a structurally impaired mouth 5
• Mouth-Airway-Sleep-Alignment (MASA) Axis: Axis: a new term introduced here to link an Impaired Mouth and many other comorbidities with SRDB as an end result.
• Clinical Epigenetics: a novel approach to diagnose and treat Impaired Mouth as the starting point of reviving sleep and airway.
The purpose is to help dental and medical professionals grow new eyes to see past 2 rows of teeth to empower oral-systemic health by mouth. Let’s begin with a dentist’s personal case.
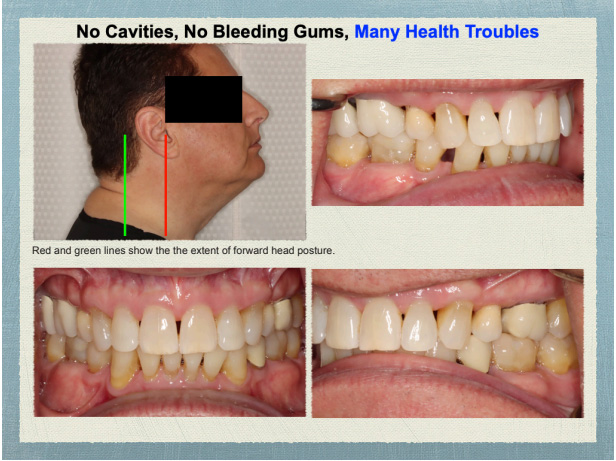
Figure 1. Photos courtesy of Dr. JB’s periodontist
The Case of Dr. JB
“I’ve managed it the best I could”: Dr. JB is a fellow dentist, age 66, and a new patient seeking to improve his current oral-systemic health if possible. His presenting complaints include:
1. CPAP intolerant, AHI of 46 tested 7/2023
2. OSA managed with Mandibular Advancement Device
3. Some daytime sleepiness
4. Bruxing + TMJ Issues
5. Asthma + Allergies since grade school
6. Stiffness L3/4 x 25 yrs managed w/ yoga
7. Atrial fibrillation treated with ablation 16 yrs ago
8. History of GERD now on Pepcid;
9. History 4 bicuspid extraction orthodontics in high school
10. Sugar addiction; Fast glucose 105.
Physical evaluation reveals no caries nor periodontal inflammation. No dental crowding with 4 first bicuspid missing. Minimal airway area on his CBCT is 104 mm2, which is barely enough to survive with struggles. What would do you do for Dr. JB, based on what’ve learned from dental school, or from taking CE? How can we better serve Dr. JB, and indeed many patients in similar plight? Managing symptoms can be costly and escalating, while finding and treating root causes is effective and de-escalating. Thus treating root cause is ultimately more cost-effective and higher order patient service.
"A HEALTHY MOUTH IS MORE THAN HEALTHY TEETH"
-US Surgeon General David Satcher-
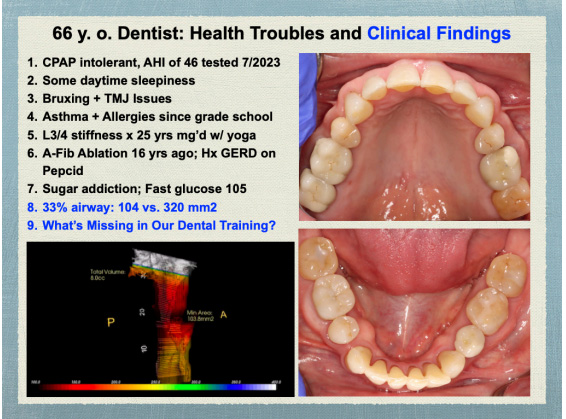
Figure 2. Impared Mouth Syndrome arising from Dr. JB's maxilla & mandible.
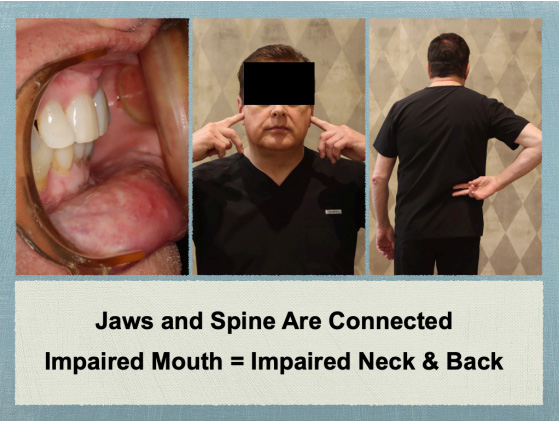
Figure 3. Pains in head, neck, and back have strong oral contributions.
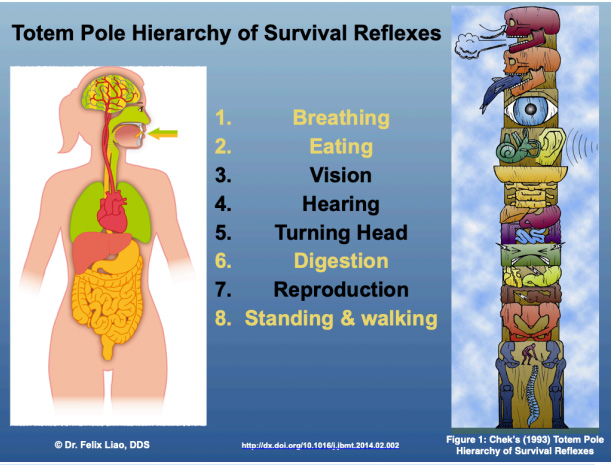
Figure 4. Inter-disciplinary agreement on the mouth’s role in whole body
health: Felix Liao’s Holistic Mouth Solutions8 and Paul Chek’s Totem Pole Hierarchy of Survival Reflexes9.
The Case of Dr. SB
So what’s a root cause of Dr. SB’s issues? This requires dentists as fixers of teeth and physicians as manager of symptoms to “zoom out” to see the role of mouth structure in whole body health.
Restore Physiology by Mouth: Discover Mouth-Airway-Sleep-Alignment Axis
Resuscitation in ER or ICU takes place at the mouth. Diabetes and obesity stem from uninformed misuse by the owner-operator. OSA can be seen as the end of a downhill slide. On its upper slope, there are many intra-oral clues, including bruxing, snoring, TMJ, abfractions, and bone loss, seen daily in dental offices.6
A whole generation of dentists have bad “smiles” and cosmetic dentistry drilled into their clinical eyes. Straight white teeth often have miserable owners with many oral systemic symptoms, as in Dr. JB’s case and others shown in Relaunch Your Vitality.7
The body is organized around the Mouth-Airway-Sleep (MAS) axis from birth on. Indeed, all of Dr. JB’s symptoms at age 66 can be traced to not knowing Impaired MASA: Mouth-Airway-Sleep-Alignment (MASA) Axis in 120 dental checkups over 60 years.
The next 2 cases will show how MASA Axis can impair whole body health of another fellow dentist and a physician, and how it can be restored. A final case study will show the details of this novel diagnosis and treatment.
Dentists & Doctors Also Suffer Impaired Mouth Syndrome Personally
“I’m living Impaired Mouth Syndrome now!” Dr. SB, a fellow dentist reached out from Canada once she learned the term. “I have severe chronic TMD, and I have done lots of chiropractic work acupuncture, massage, and even trigger point injections for it. I also suffer from facial asymmetry, fatigue, typical poor posture of a dentists, restricted airway in my nose…, and teeth grinding."
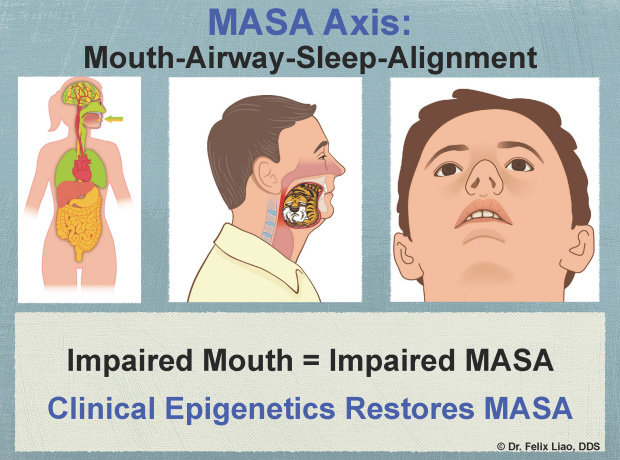
Figure 5. Impaired Mouth Syndrome is undiagnosed in over 90% of dental patients, in this author’s experience.
Why are dentists suffering from undiagnosed Impaired Mouth Syndrome? Where should we start with a patient like this, whether you are an airway dentist or sleep physician? My answer: connect the dots from every and all presenting complaints to an Impaired Mouth. This is done with:
A. Airway diagnostic records, including photos, CBCT, models, medical-dental history from birth to now, and physical evaluation from head to feet.
B. Diagnosis of skeletal malocclusion: identify which of the 3 dimensions are off that can account for her symptoms physiologically.
C. Treatment plan addressing
- Impaired Mouth Structure: including but not limited to deficiency/excess in maxilla or mandible, airway volume and minimal area (where airway collapses. tongue-tie, incompetent lip seal, abnormal swallow,
- Structures associated with the mouth: postural chain from head to feet, nasal and sinus cavities, cranio-facial skeleton, internal systems regulating hormones, circulation, stress response, digestion, nutrition, lifestyle, weight and obesity management, etc., as indicated individually
- Multi-disciplinary referrals and collaborations to restore physiology.

Figure 6. Epigenetics is the different dental-facial appearance of the same person Dr. SB.
Let’s now focus on the breakthroughs that can come from seeing Impaired Mouth Syndrome and correcting impaired Mouth10-Airway-Sleep-Alignment Axis, leaving diagnostics details to later.
Dr. SB’s treatment began with an epigenetic oral appliance paired with a bone-building diet. Epigenetics is, “the study of how behavior and environment can change how genes work”, according to according to Center for Disease Control and Prevention.10 Thus epigenetics is a radical departure from classical orthodontic mechanics.
Treatment with clinical epigenetic include a bone building- diet paired to an epigenetic appliance capable of growing the maxilla in adults 11, 12, and improved facia development beyond orthodontic mechanics 13, 14
Epigenetics is the difference between classical appliance mechanics and Dr. SB’s transformation in 12 months as shown in Figure 6.
Subjective Units of Distress Scale (SUDs) is a valid assessment tool 15 used in psychology using a 0-10 scale by patient subjects, with 10 being “feels unbearably bad, beside yourself, out of control, overwhelmed, at the end of your rope”16
Note in Figure 7:
• Distress is subjectively felt (thus no absolute precision is needed),
• The score reflects feeling of the moment.
• Bodily tension and physical pain indicate a higher subjective distress.
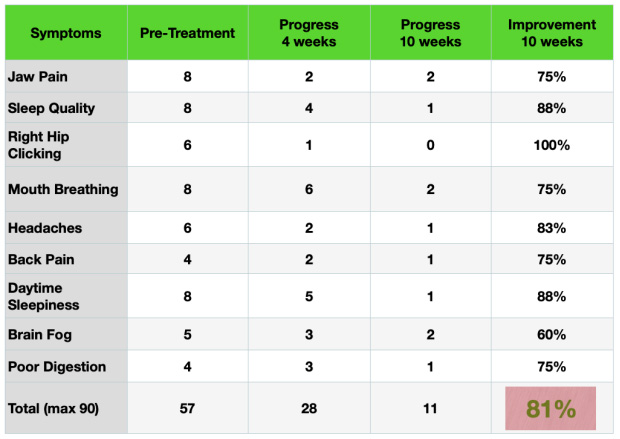
Figure 7: Symptom Progress Tracker using Subjective Units of Distress.
This 81% improvement is remarkable in several ways:
1. All symptoms improved, whether dental, medical, or cerebral (sleep quality, brain fog), which reflects on the mouth’s multiple physiological functions.
2. Many diverse symptoms stemming from a structurally impaired mouth can be improved with Impaired Mouth diagnosis and epigenetic oral appliance.
3. Epigenetics can work in a 43 year-old (thus in all adults) with sound teeth.
4. Epigenetics does not involve invasive injection, drilling, or surgery, nor pain.
5. Rapid and effective iimprovement: 50% in 4 weeks.
Symptoms will persist when root-cause(s) are unknown or ignored. Similarly, symptoms will improve if Impaired Mouth is correctly diagnosed and treated as a root cause. An oversimplified summary of Impaired Mouth diagnosis and treatment is shown in Figure 8.
Not all appliances are created equal. Done right, pain fafes in days and weeks, while fatigue may take months to pay off the oxygen debt. Recovery rate can vary depending on symptom chronicity, severity, biological age, and remaining vitality.
"NOT ALL SLEEP APPLIANCES ARE CREATED EQUAL"
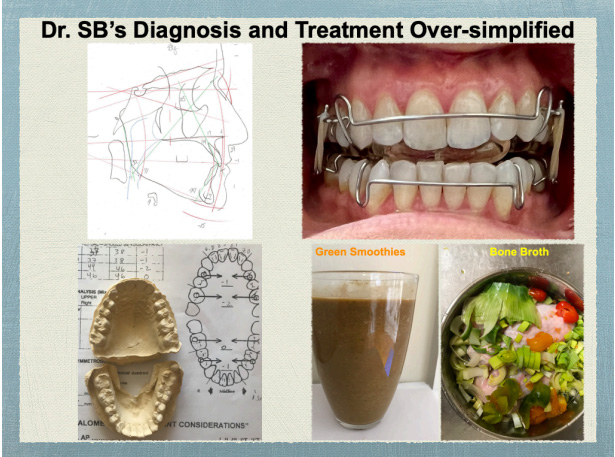
Figure 8. Left Dr. Liao’s 3D Jaw Diagnostics® method for designing
epigenetic oral appliance and bone building diet (right). The elastics are
optional to help prevent retrusion and thus pain and fatigue.
A correctly prescribed oral appliance based on 3D Jaw Diagnostics® method, plus body work and diet change as needed, can do wonders for airway, sleep, headache, back pain, fatigue, and more. This takes significant additional training beyond traditional teeth-centered dentistry.
Physicians Too Suffer from Impaired Mouth Syndrome Undiagnosed
Physicians who are not dentists are just as susceptible to having Impaired Mouth Syndrome undiagnosed as average dental patients. Most readily admit the mouth is one big hole in their medical training.
Dr. AR, a highly specialized surgeon, had to reduce her workload due to severe jaw pain, migraines, sleep apnea, and brain fog. Her hands were ice-cold when I evaluated her, suggestive of hypothyroidism. Her health history included multiple medications, plus
• Lots of dental work for wear & tear from teeth grinding and dentinal exposure and sensitivity from gastro-esophageal acid reflux, Orthodontics twice as a teen and in mid-30’s (a big red flag for Impaired Mouth undiagnosed).
• Nasal and jaw surgery with minimal improvement in her sleep and jaw pain— see the hardware in Figure 9
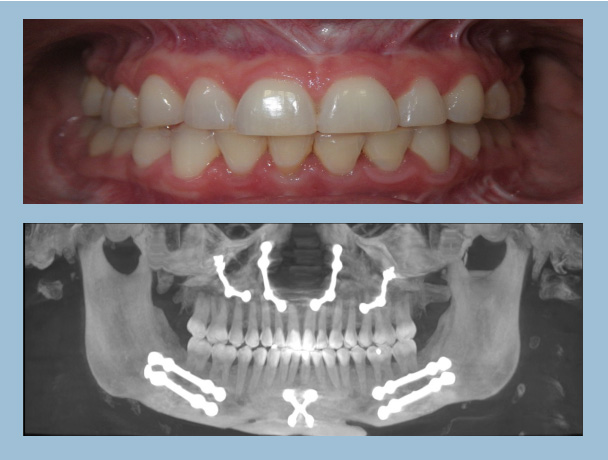
Figure 9: Straight white teeth in a miserable physician owner
The Case of Dr. AR
Dr. AR had her 3D Jaw Diagnostics worked up started treatment as describe earlier, and her progress is shown in Figure 10.
70% was Dr. AR’s gain in 4 months. Can an Impaired Mouth be huge in overall health? Dr. Rich Beistle’s words are worth repeating here: “You see only what you know, hence you can’t diagnose what you don’t know.”
With the hind sight of Impaired Mouth diagnosis, all of Dr. AR’s prior dental treatments missed her Impaired Mouth as an oral-systemic liability. This missed diagnosis comes at a tremendously high cost financially, physically, and emotionally. Our patients deserve better.
Impaired Mouth’s Global Shadow
Dental patients have medical issues, and medical patients have dental issues, and both have frequent mood issues. Most patients still do not feel well despite having seen many doctors and dentists and leaving with “good” checkups. DM, an entrepreneur age 35, is a case in point that knowing Impaired Mouth Syndrome and Mouth-AirwaySleep-Alignment Axis can create breakthrough outcomes.
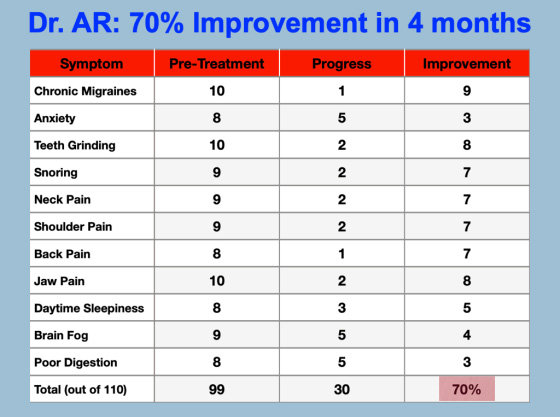
Figure 10: Note Dr. AR’s symptoms range across medical, dental, and cerebral nature.
The Case of Dr. DM
DM came with CPAP intolerance, prescribed medications for attention deficit and insomnia, plus a list of symptoms that worried his wife:
• Witness apnea for two years,
• Teeth grinding despite using night guard,
• Progressively crowding and chipped teeth,
• Fatigue: “I’m so tired”
• Anxiety, periodic limb movement, PTSD,
• Pain in neck shoulders and back,
• Wake up refreshed 0 days a week “since forever”
• Poor memory: “I can’t convert short-term memory into long term.”
His sleep doctor could not help him, nor his MDs. Their training did not include Impaired Mouth Syndrome. Dentally, DM has no caries, no periodontal pockets beyond 3 mm, good attached gingiva, no bleeding on probing, and his teeth looked straight and clean. Yet the key to his issues is right there in his mouth!
Diagnosing Oral Contributions to Systemic & Dental Issues
Physical evaluation reveals strong mandible retrusion to achieve posterior intercuspation. This mandibular retrusion drives the tongue further into DM’s pharynx to aggravate his airway-related symptoms. It can also lead to TMJD and associated neckshoulder-back pains prominent his DM’s presenting complaints.
Airway diagnostic records were taken and they reveal the following as shown in Figure 12:
1. Case documentation concludes photos, CBCT, models, medical-dental history from birth to now, and physical evaluation from head to feet.
2. Sassouni Plus Cephalometric analysis17, 18, 19, 20, 21:
- Maxilla is retruded relative to Nasion by -5 mm
- Mandible is retruded relative to maxilla by -5 mm, which means DM has class-II skeletal malocclusion)
- Skeletal vertical is + 15 mm with steep mandibular plane angle indicative of a history of nasal obstructioninduced mouth breathing.
3. Model analysis22: Maxilla is not wide enough for maxilla to fit into
- Maxilla is -6 mm between first premolars and -1 between first molars.
- Mandible is -2 between first premolars and -1 between first molars.
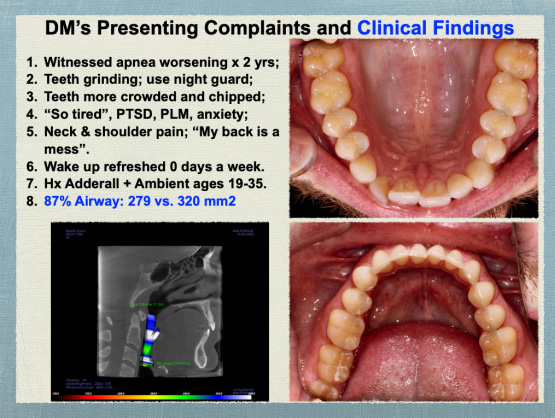
Figure 11. DM’s airway is far better than most OSA cases, yet his symptoms say it’s not enough.
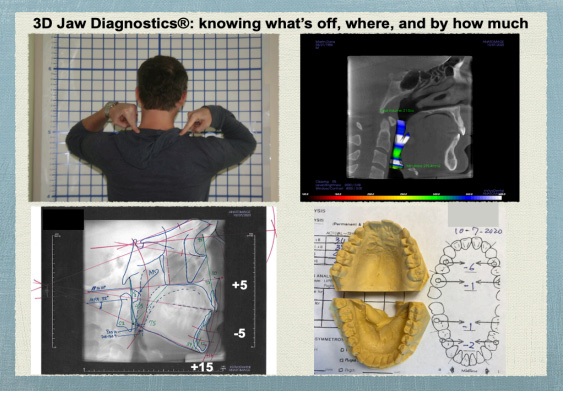
Figure 12. 3D Jaw Diagnostics® is a trademarked method to assess the space
between maxilla and mandible that serves as “home office” for the tongue. It reveals where and how much the jaws are deficient or excessive, and aids in
target treatment with custom-deigned epigenetic oral appliances.
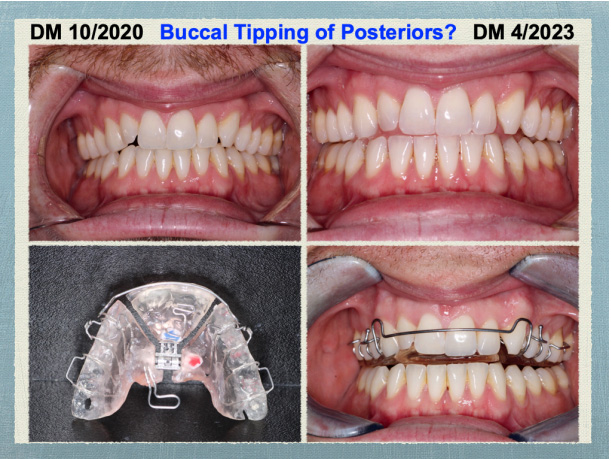
Figure 13. Counter-clockwise from top left: Pre-treatment, epigenetic oral
appliance outside and in place, and end of Phase-I appliance treatment without clear aligners or orthodontics.
This “crime scene investigation” reveals the true culprit to be habitual mouth breathing and deficient maxilla in DM’s case: -5 saggitally, -6 transversely. 3D Jaw Diagnostics® is a method to
A. Identify which of the three dimensions are off, and by how much,
B. Design epigenetic appliance based on each individual’s cephalometric data
C. Grow maxilla and mandible in combination with a bonebuilding diet 23
Construction bite is taken to promote gene expression in condylar gene expression 24. Figure 13 shows the result of this diagnostic workup and this diagnostic workup and Clinical Epigenetics treatment in 30 months later.
Note:
• The midlines are aligned compared to pre-treatment,
• No buccal tipping of posterior teeth in the upper right image.
But why is the maxilla deficient? Tongue-tie is one answer. This is seen in lower right image in Figure 1. Myofunctional therapy (MFT) in combination with laser release is indicated. While MFT can improve AHI by 50% in adults and 62% in children 25, I prefer to do MFT at or near the end of Phase I appliance therapy when the oral space is sufficiently regrown for the tongue to “exercise” with ease.
Figure 15 shows the diagnosis and treatment outline, while Figure 16 shows the anterior view of DM’s occlusion and the Epigenetic maxillary appliance used.
The result of said Phase-I epigenetic appliance treatment is shown in Figures 17.
Figure 18 shows the transverse gains after 30 months:
• Maxilla width: 8 mm anteriorly and 6 mm posteriorly
• Mandible width : 4 mm anteriorly and 4 mm posteriorly
• Room for maxillary anterior teeth to align with clear trays

Figure 14 Note absence of buccal tipping in posterior teeth the
tongue is a major obstructor in obstructive sleep apnea.
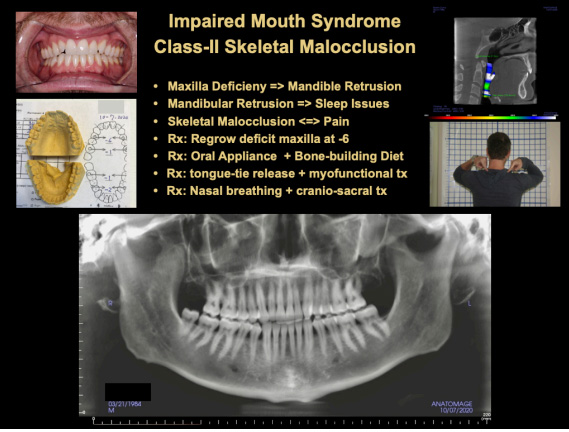
Figure 15 Note absence of buccal tipping in posterior teeth
sound treatment begins with sound diagnosis.
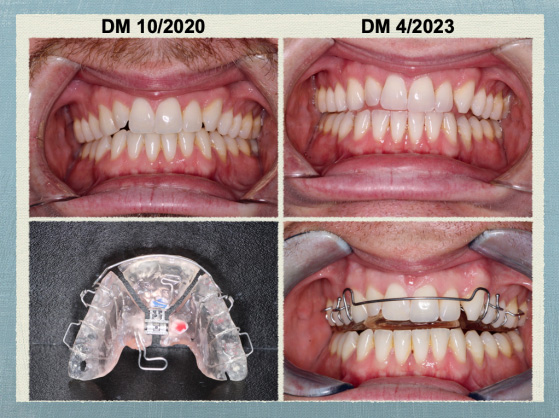
Figure 16. Note absence of buccal tipping posteriorly after 3 years and 3
maxillary appliances.
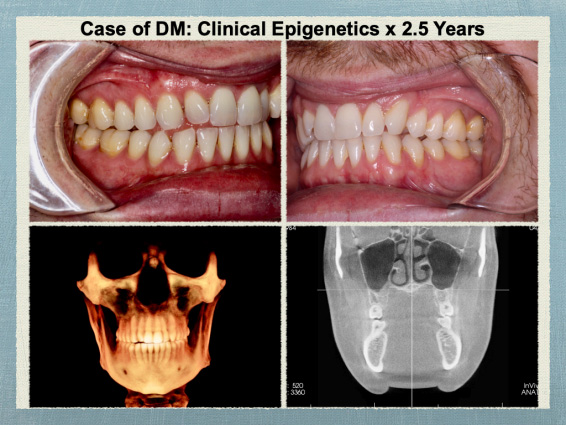
Figure 17 note absence of buccal tipping in posterior teeth in all 4 images.
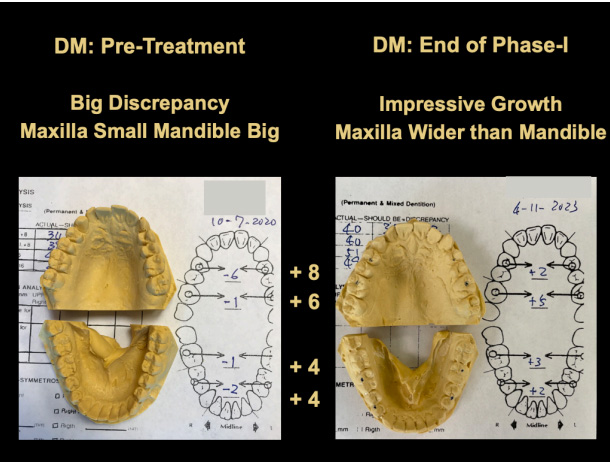
Figure 18. End of Phase-I Jaw-centered Orthopedics, before Phase II Teeth-
centered Orthodontics.
Figure 19: shows 61% gain in airway volume after three maxillary appliances and one mandibular. This is epigenetic growth and redevelopment not possible with orthodontic movement or buccal tipping.
Figure 20 shows DM’s cephalometric changes from skeletal Class II to Class I, and skeletal vertical gains 8 mm. The unchanged upper incisal angle will be treated in Phase-II orthodontic clear aligners.
Figure 21 shows 90% improvement in DM’s Impaired Mouth symptoms using Subjective Units of Distress scale of 0-10. Again, the gains happen across medical, dental, and mood lines. And they are accomplished simply with epigenetic redevelopment of an Impaired Mouth, without the usual pain and other side effects typically associated with dental or medical care.
Summary: In the 3 cases presented, we can see:
A. Impaired Mouth leads to a wide range of medical, dental, and cerebral symptoms known as Impaired Mouth Syndrome.
B. Knowing Impaired Mouth Syndrome is the start of diagnosis and treatment at the root-cause level.
C. 70-90% of presenting complaints can be improved with treatment using epigenetic oral appliance designed with 3D Jaw Diagnostics in combination with a bone building diet and inter-disciplinary collaboration.
D. Improvement is rapid and interdisciplinary without resorting to medication, surgery, or cutting teeth with dental drills, nor braces:
- 81% in SB in 10 weeks
- 70% in AR in 4 months
- 90% in DM in 30 months
These case studies illustrate the potential impact of dentists and physicians trained in the recognition of impaired MASA Axis and epigenetic treatment of Impaired Mouth Syndrome.
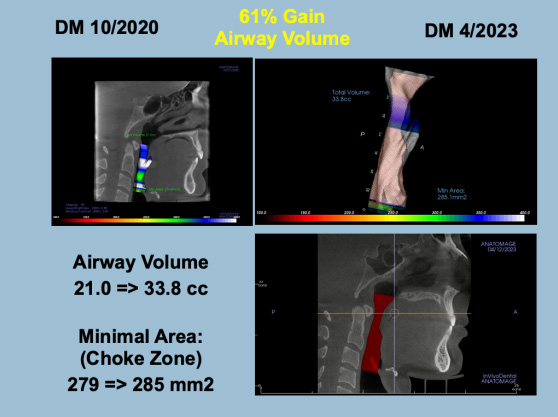
Figure 19 Upper left image is pre-treatment, while upper and lower right image is end of Phase-I appliance treatment.
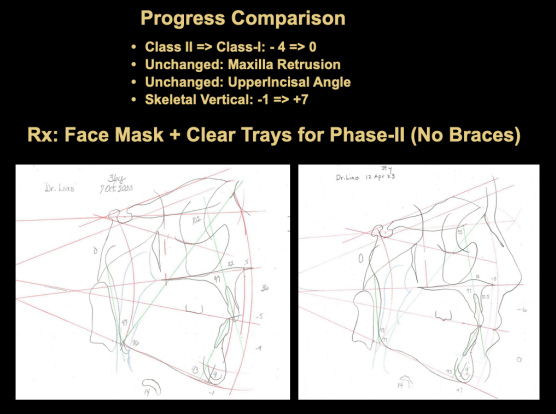
Figure 20 Major improvement in cephalometric landmarks pre-treatment and end of Phase-I.
"THERE’S AN EPIDEMIC OF IMPAIRED MOUTH, YET WE RECEIVED ALMOST ZERO EDUCATION IN MEDICAL SCHOOL. PATIENTS CANNOT POSSIBLY KNOW ABOUT IMPAIRED MOUTH IF THEIR DOCTORS DON’T"
- Dr. Ar on Her Experience as a Patient -
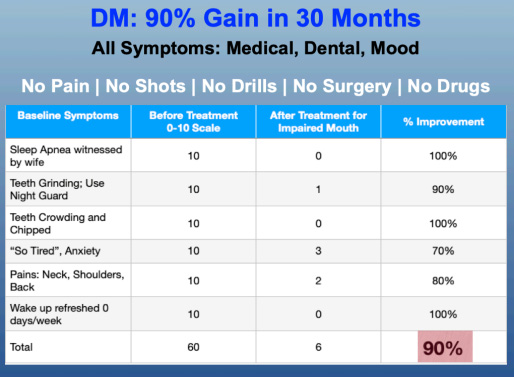
Figure 21. Breakthroughs from diagnosing Impaired Mouth Syndrome and
restoring Mouth-Airway-Sleep Axis.
Figure 22. Seeing Impaired Mouth Syndrome and Mouth-Airway-Sleep Axis
can lead to breakthrough outcomes using 3D Jaw Diagnostics and clinical epigenetics.
Conclusion
70-90% of presenting complaints either resolved or improved in the three cases presented. Symptoms in the breakthroughs are broad across interdisciplinary lines. Treatment uses a novel clinical epigenetic approach without the usual pain or side effects associated with traditional dentistry, surgery, or medications.
“Epigenetics has recently evolved from a collection of diverse phenomena to a defined and far-reaching field of study”, states National Institute of Health.27 The cases presented illustrate the medical, dental, mental, and mood benefits of applying epigenetics to oral environment in practice by properly trained airway dentists and oral behavior at home by compliant patients.
Diagnosis starts with recognizing Impaired Mouth Syndrome and seeing that health and wellness revolves around the newly coined Mouth-Airway-Sleep-Alignment Axis. This has significant implications in personal and societal terms: “OSA has been associated with many of the most common health conditions causing morbidity, mortality, social and economic cost. Most data suggest that the costs of treating OSA are less than the human and economic cost of untreated OSA”, states a 2020 article in New Frontiers in Sleep Disordered Breathing.26
While no treatment is far more costly in the long run than the cost of root-cause treatment, wrong treatment and missed diagnosis escalate cost through harm and irreparable loss, as in the case of Dr. JB shown early in this article. Surgeon AR still had a severe case of Impaired Mouth Syndrome after paying for her fullmouth dentistry and jaw surgery.
What awareness was missing in the dentists trusted by Drs. AR, SB, and JB? “There’s an epidemic of Impaired Mouth, yet we received almost zero education in medical school. Patients cannot possibly know about Impaired Mouth if their doctors don’t”, reflects Dr. AR on her experience as a patient.
Teeth-centered dentists excel at restoring diseased teeth. Without downplaying traditional dentistry’s foundational importance, our patients face a critical need for Impaired Mouth diagnosis today. Becoming an airway-centered mouth doctor can restore miserable patients by reviving impaired Mouth-Airway-Sleep-Alignment Axis.
“Pediatric obstructive sleep apnea in non-obese children is a disorder of oral-facial growth.”28 This means sufficient oral facial growth employing clinical epigenetics can be a proactive strategy to counter that downhill slide toward OSA.29 Getting trained on seeing Impaired Mouth Syndrome and clinical epigenetic solutions is the first step.
References
1. Lyons, M. J., Bhatt, N. Y., Pack, A. I., & Magalang, U. J. (2020). Global burden of
sleep-disordered breathing and its implications. Respirology, 25(7), 690-702. https://
doi.org/10.1111/resp.13838
2. U.S. Department of Health and Human Services. Oral Health in America: A
Report of the Surgeon General. Rockville, MD: U.S. Department of Health and
Human Services, National Institute of Dental and Craniofacial Research, National
Institutes of Health, 2000.
3. American Dental Association, The Role of Dentistry in the
Treatment of Sleep Related Breathing Disorders: https://
www.ada.org/-/media/project/ada-organization/ada/ada-org/files/ resources/
research/the-role-of-dentistry-in-sleep-related-breathingdisorders.pdf
4. Cole J, Sleep-Related Breathing Disorders: The Role of the
Dentist. Special Section, Dental Sleep Practice: https://
dentalsleeppractice.com/ce-articles/special-section-sleep-relatedbreathing- disorders-
the-role-of-the-dentist/
#:~:text=The%202017%20ADA%20Policy%20Statement,may%2 0lead%20to%20
airway%20issues.
5. Liao, F. Licensed To Thrive: A Mouth Owner’s GPS to Vibrant Health & Innate
Immunity. Crescendo Publishing 2021, p. 19-31.
6. Liao, F. Early Sirens: Critical Health Warnings & Holistic Mouth 35 Solutions for
Snoring, Teeth Grinding, Jaw Clicking, Chronic Pain, Fatigue, and More. Crescendo
Publishing 2017.
7. Liao, F. Relaunch Your Vitality: Root Out Chronic Pain & Fatigue to Enjoy Life
Again. Holistic Mouth Solutions, 2023.
8. Liao, F. 6 Foot Tiger 3 Foot Cage: Take Charge of Your Health by Taking Charge
of Your Mouth. Crescendo Publishing 2017.
9. Macphail K, the Hierarchy of Survival Reflexes: A Summary of Evidence. Kieran
Macphail’s blog.
10. Centers of Disease Control and Prevention: What Is Epigenetics? Accessed August
27, 2023.
11. Singh GD, et al, Mid-facial development in adult obstructive sleep apnea. Dent.
Today, 30(7), 124-127, 2011.
12. Liao F, Singh GD: Resolution of Sleep Bruxism Using Biomimetic Oral Appliance
Therapy, A Case Report. J. Sleep Disorder Therapy 2014, 4:4.
13. Liao, F. Your Child’s Best Face: How to Nurture Top Health & Natural Glow.
Holistic Mouth Solutions, 2022.
14. Liao, F. Clinical Epigenetics: Solutions for “Head-Scratcher” Issues in
Orthodontics. J. Am. Orthodontic Society, Summer 2023, p. 12-23. http://jaos.
orthodontics.com/archive/? m=4034&i=799327&p=12&p1=4034&ver=html5
15. Wolpe, Joseph (1969), The Practice of Behavior Therapy, New York: Pergamon
Press, ISBN 0080065635) PMID: 20509987
16. Wikipedia: Subjective Units of Distress Scale
17. Sassouni, V. A Roentgenographic cephalometric analysis of cephalometric-facto-
dental relationships. AJO-DO Volume 41, ISSUE 10 p.735-764, OCTOBER 1955.\
18. Beistle, Richard T.: A Comprehensive Cephalometric System for Diagnosis and
Treatment Planning in Functional therapy. The Functional Orthodontist, Vol. 1, No.
1: 39-48, 1984. 19. Beistle, Richard T.: Simplified Sassouni Plus: An Update. The
Functional Orthodontist, Vol. 4, No. 3:12-17, 1987.
20. Gerber, Jay W.: TMD Waning Sign: Cephalometrics, The
36 Functional Orthodontist, AAFO, Vol. 11, No.2, pp 15-19, March/ April 1994.
21. Magill, TS: Functional Forum: More Meaningful Cephalometrics The Functional
Orthodontist, AAFO, Vol. 11, No. 5, p 38-41, Sept-Oct, 1994.
22. Schwarz Model Analysis (2006): https://www.smlglobal.com/sites/default/
files/1PBB20.pdf
23. Liao, F. Licensed To Thrive: A Mouth Owner’s GPS to VibrantHealth & Innate
Immunity. Crescendo Publishing 2021. Chapter
23. Liao, F. Licensed To Thrive: A Mouth Owner’s GPS to Vibrant Health & Innate
Immunity. Crescendo Publishing 2021. Chapter
24. Fuentes MA, et al, Lateral functional shift of the mandible: Part II. Effects on gene
expression in condylar cartilage. Am J Orthodontics and Dentofacial Orthopedics
2003;123:160-6.
25. Camacho M, Certal V, Abdullatif J, Zaghi S, Ruoff CM, Capasso R, Kushida
CA. Myofunctional Therapy to Treat Obstructive Sleep Apnea: A Systematic Review
and Meta-analysis. Sleep. 2015 May 1;38(5):669-75. doi: 10.5665/sleep.4652. PMID:
25348130.
26. Lyons, M. J., Bhatt, N. Y., Pack, A. I., & Magalang, U. J. (2020). Global burden of
sleep-disordered breathing and its implications. Respirology, 25(7), 690-702. https://
doi.org/10.1111/resp.13838
27. Goldberg AD, Allis CD, Bernstein E. Epigenetics: a landscape takes shape. Cell.
2007 Feb 23;128(4):635-8. doi: 10.1016/ j.cell.2007.02.006. PMID: 17320500.
28. Huang YS, Guilleminault C. Pediatric obstructive sleep apnea and the critical
role of oral-facial growth: evidences. Front Neurol. 2013 Jan 22;3:184. PMCID:
PMC3551039.
29. Liao, F. Clinical Epigenetics: Solutions for “Head-Scratcher” Orthodontic Issues.
Journal of American Orthodontic Society, Summer 2023, p. 12-23: http://jaos.
orthodontics.com/archive/? m=4034&i=799327&p=12&p1=4034&ver=html5
For more information, please visit
https://holisticmouthsolutions.com/
Or you can email directly to