Need Assistance? Call us today! 602-478-9713
Obstructive sleep apnea is a a lifetime disorder that requires the clinical team to plan long term and treat the whole patient. The literature and more importantly medical insurance providers urge careful evaluation of temporomandibular joint as a part of oral appliance clinical work up. I read the following article by Dr. James Fricton, which was previously published in the CDA journal, and I really got excited about his approach.
This comprehensive Patient focused program seems to be exactly what the sleep apnea dentistry world needs to continue to grow. We have added some diagnostic and thereapeutic protocols and started to move away from single treatment protocols with combination therapy etc. Over the last 6 years surface EMG and the calculation of Bruxism Episodes Index (BEI) has become much more routine in the evaluation of sleep disorders and jaw parafunction. In my opinion the management of sleep disorders is much more a disease state management program that the application of a specific therapy without the comprehensive individualized management plan. Dr Fricton makes the excellent point that Clinicians tend to see what they treat and treat what they see.
![]() Clinicians tend to see what they treat and treat what they see. Clinicians who see a stress etiology treat with stress management; surgeons who see a joint pathology treat with surgery; and dentists who see a dental etiology treat the teeth. As a result, treatment success is often compromised by limited approaches that address only part of the problem
Clinicians tend to see what they treat and treat what they see. Clinicians who see a stress etiology treat with stress management; surgeons who see a joint pathology treat with surgery; and dentists who see a dental etiology treat the teeth. As a result, treatment success is often compromised by limited approaches that address only part of the problem ![]()
There are innovations in the field that have come along recently such as the Quick Splint which give the clinician a wonderful tool to increasing speed to treat considerations and at low cost. Please take the time to read over Dr Fricton's article and let me know what you think.- ed
Temporomandibular Disorders: A Human Systems Approach
James Fricton, DDS, MS
ABSTRACT
The face and associated cranial,oral and dental structures are among the most complicated areas of the body, contributing to an array of common orofacial disorders that include temporomandibular disorders (TMD), orofacial pain disorders and orofacial sleep disorders. This paper presents a broad, inclusive approach to diagnosis and management of TMD that reflects both conceptual models of human systems in understanding chronic illnesses as well as systematic reviews of treatment for successful management.
The face and associated cranial, oral and dental structures are among the most complicated areas of the body, contributing to an array of orofacial disorders, including temporomandibular disorders (TMD), orofacial pain disorders, orofacial sleep disorders, oral lesions, dental disorders and oromotor disorders. Orofacial pain disorders are the most common of these problems and can cause symptoms of orofacial pain, jaw dysfunction and chronic head and neck pain, with a collective estimated prevalence of at least 20 percent of
the general population (TABLE 1).1-7 To complicate matters, oral and craniofacial structures have close associations with the functions of eating, communicating, seeing and hearing, and they form the basis for appearance, self-esteem and personal expression and, thus, can deeply affect an individual’s psychological and functional status.7 A national poll found that adults working full time miss work because of head and face pain more often than for any other site of pain.5
The high prevalence, personal impact and poor access to care for these problems have led to an expanded role for dentistry in providing solutions. However, because dentists focus most of their patient care on treatment of the dentition and related structures, it can be a challenge to understand the broader scope of diagnosis and management of these conditions. Treatment of TMD, like many pain conditions, is often singular and can vary according to the clinician’s favorite theory of etiology. Clinicians tend to see what they treat and treat what they see. Clinicians who see a stress etiology treat with stress management; surgeons who see a joint pathology treat with surgery; and dentists who see a dental etiology treat the teeth. As a result, treatment success is often compromised by limited approaches that address only part of the problem.
This paper summarizes a broader, more inclusive philosophy in diagnosing and managing TMD that reflects both new conceptual models in understanding chronic illnesses as well as systematic reviews of therapeutic strategies for successful management of TMD.
Human Systems Theory: A Comprehensive Model for Understanding Chronic Illness
Humans are complex, multidimensional and dynamic and live within an ever- changing physical and social environment. Yet our traditional biomedical model is based on a scientific paradigm that is unidimensional, reductionist and in exible because it is based primarily on understanding the underlying pathophysiology. While distinct pathophysiological mechanisms occur in all chronic conditions, understanding the multitude of factors that play a role in the onset, perpetuation and progression of the illness is the key to successful management.8 Thus, traditional scientific protocols often fall short in providing an adequate framework for explaining, predicting and influencing chronic illness and its outcomes. Scientific and clinical communities have been searching for a more flexible, holistic and integrated model that describes the changes in human biology that can occur in response to the circumstances in our lives which contribute to the balance between health and illness.
Human systems theory (HST) provides this framework.8 As originally stated by Aristotle in 300 BC, “The whole is greater than the sum of its parts.” HST stems from research in general systems theory and originated in ecology out of the need to explain the interrelatedness of organisms in ecosystems.8-10 While conventional biological theories view the subject as a single entity, HST
views a person as a whole with an interrelationship between the subparts of his or her life. These subparts are not static but rather are dynamic, evolving and interrelated processes. The practical application of HST to patient care requires that we understand basic HST principles as they apply to the development and alleviation of illness. These include:
■ Seeing the whole patient through the eyes of the biopsychosocial medical model.8-10
■ Understanding recursive feedback cycles using cybernetics.11,12
■ Seeing the broad cumulative impact of small changes using chaos theory.13-15
■ Understanding the power of positive action through positive psychology and behavioral medicine to enhance health as part of the treatment of illness.16-19
These concepts provide a new model for understanding TMD and its management that is well founded in theory and science. It is beyond the scope of this paper to present an in-depth discussion of each concept. However, for those interested in reading further, the concepts are presented in a more creative format than traditional academic texts — i.e., as a murder mystery novel — as well as part of a University of Minnesota massive open online course (MOOC)
at coursera.org/course/chronicpain. 20
The biopsychosocial medical model was first proposed by Engel in 1977 and suggested that to understand health and illness, one needed to look at the whole person and not simply at physical pathophysiology.8-10 It recommended that we “see the big picture” of illness. Most studies of risk factors and protective factors suggest that each person has a unique set of interrelated factors that can either perpetuate or protect from an illness, including TMD. These contributing factors correspond to each realm of our lives, including the mind, body, emotions, spirituality, lifestyle, social relationships and the physical environment (FIGURE 1).
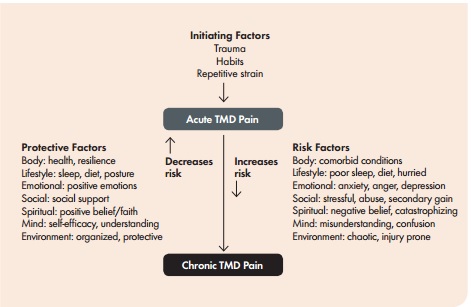
FIGURE 1. Multiple protective and risk factors play a role in the progression from acute to chronic TMD pain.
By improving them, the strategies for management have greater success than the sum of any individual treatment directed at one realm. Cybernetics, a concept defined in physics, was first applied to human systems by Bateson in 1978.11,12 It suggests that “what goes around comes around” and each element of a system generates a change, which causes feedback to the entire system. Positive feedback triggers a continuation of the cycle, while negative feedback leads to its discontinuation.
This is often referred to as a self-reflexive or “circular causation” relationship. Positive and negative feedback cycles
play an important role in sustaining a person’s illness over time (FIGURE 2).
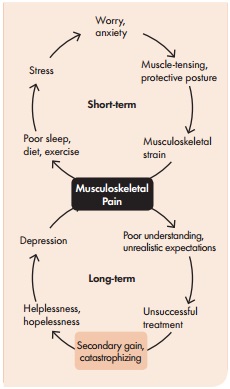
FIGURE 2. Positive and negative feedback cycles play an important role in sustaining a person’s illness over time.
Patients with an illness often fall into the recursive cycles that perpetuate the illness. Contributing factors to an illness, such as repetitive strain, depression or poor sleep, are elements that sustain the cycle. Several types of change can influence these cycles (FIGURE 3).
First-order change is based on “reinforcement” of existing elements that promote maintenance or escalation of the existing cycle and its related illness. A second-order change involves a “revelation” that makes a significant change from within the system through multimodal education, training and treatment that lead to a new state. This change may either be toward improved health or escalation of the illness, depending on the direction of change in the element. Finally, a third-order change is based on “enlightenment,” which produces a change from outside to achieve a new level of existence distinctly different from the original structure. Second- or third- order changes are the basis for significant improvement of a condition to create a new paradigm for the health of the individual.
Small first-order compensatory changes made by a patient in response to TMD pain, such as reducing use of the jaw, taking an analgesic or other self care, can improve the illness if it is an acute self-limiting problem, at least in the short term. However, these compensatory changes may also allow a more complex illness to fall into a long-term chronic cycle (FIGURE 2). If a clinician can help a patient make higher order changes by understanding the multiple elements in the cycle and changing those keystone factors that perpetuate it, the illness may change more readily. Integrative care strategies that encourage second- order change within an existing cycle include splints, physical therapy and behavioral management of oral habits, sleep and muscle tension. This strategy works quite well for simple to moderate cases, but more complex patients may need a more robust intervention. In those cases, transformative care strategies encourage third-order changes that can lead to the most dramatic long-term results.
Third-order change involves not only treatment of the TMD pain as noted, but also working with a team to identify all co morbid conditions and contributing factors and helping the patient make major changes to factors that may be perpetuating the long-term cycles. These changes could include managing a co morbid medical condition such as fibromyalgia, addressing stressful or abusive relationships and changing poor work situations. In this way, healthier, positive feedback cycles are set up that do not perpetuate the factors that drive the illness. Chaos theory was first popularized by Lorenz (1963) in a paper on the theories of diverse weather patterns entitled “Does the Flap of a Butterfly’s Wings in Brazil Set off a Tornado in Texas?” He presented evidence that small differences in initial conditions of a system might yield widely diverging outcomes within dynamic systems. Chaos theory suggests that “it’s the little things that matter the most.” When applied to health and disease, it suggests that multiple risk factors can each play a small role at early stages of a chronic illness. However, when these factors are combined, they will accelerate the condition dramatically.
As FIGURE 4 illustrates, an illness begins with initiating factors such as acute physical injury of the muscles and joints. In most cases, this pain is transient and resolves without complication or persistence. However, if a sufficient number of contributing factors are present, even though small, the balance can shift from healing of acute pain to delayed recovery and chronic pain (FIGURE 2).44-50 Various underlying neural mechanisms, such as peripheral and central sensitization and wind-up, play a role in this process that is difficult to predict. Likewise, the presence of protective factors and early intervention in multiple factors will have the greatest impact in resolving the condition.
Behavioral medicine, then, suggests that specific behavioral interventions such as exercise and oral habit reversal can help restore health and wellness. It complements theories on positive psychology that focus on building health, strength and positive virtues as much as on correcting illness, problems and vices.16,17 The Aristotelian idea that we are what we repeatedly do is supported by much research in achieving health and wellness.
These theories explain the diverse results of placebo-controlled clinical trials for TMD pain and other pain conditions which suggest that many different interventions, from splints and medications to physical and cognitive-behavioral therapies and even injections and surgery, can all be used to alleviate TMD pain.21-39 The effect of each of these interventions beyond the placebo effect may be small, but they are all significant. Furthermore, by combining these concepts in a multimodal integrative model of care that is based
on a human systems approach, the small effects of multiple interventions employed at the same time can result in the greatest positive outcomes. Thus, the evaluation and management approaches proposed
in this paper follow these principles.
Principles of Evaluation
The principles of HST can be applied to the evaluation of patients with TMD
by employing an inclusive problem list, determining the complexity of the case and following the decision tree for increasing the potential for successful management.
Determine the Problem List. HST expands the traditional “problem list” to include both the physical diagnoses and the contributing factors in each realm. The physical diagnosis is the physical problem that is responsible for the chief complaint and associated symptoms. The orofacial pain disorders noted in T A B L E 1 are included in this definition of the scope of dental practice because they have characteristics that involve the oral cavity, maxillofacial area and/or the adjacent and associated structures. Contributing factors include those that initiate, perpetuate or result from the disorder but in some way complicate the problem.
These risk and protective factors are diverse and involve the seven
realms of our lives:40-63 the physical (physiologic, genetic, molecular); lifestyle (repetitive strain, posture, lifestyle, eating, sleep); emotional (depression, fear, anxiety, anger); social (relationships, abuse, secondary gain); cognitive (attitudes, understanding, honesty); spiritual (faith, beliefs, purpose); and environmental (accidents, pollution, disorganization, hygiene).
Specific risk factors for chronic pain may include peripheral factors such as repetitive strain, oral and postural habits, central mediating factors such as anxiety and depression, and comorbid conditions such as fibromyalgia, somatization and catastrophizing. Protective factors reduce vulnerability to chronic pain. These factors, which include the level of coping, self-efficacy, patient beliefs (e.g., perceived control over pain, belief that pain is a sign of damage) and social support, can also affect outcomes.
Determining Complexity. The level of care for patients can also vary considerably depending on whether their condition is simple or complex. Patients with complex TMD often present with a frustrating medical and dental situation, which may include persistent aggravation of pain, multiple clinicians, long-term medications, repeated health care visits and an ongoing dependency on the health care system. Successful management of these patients is enhanced if the level of complexity is determined and matched to the complexity of the treatment strategy. Singular treatment strategies such as
self care, physical therapy or splints can be quite successful with simple patients who have few contributing factors, but these treatments often fail in complex patients because of the chronic nature of the disease, central sensitization and long-standing maladaptive behaviors, attitudes and lifestyles.
Decision Tree for Triaging Patients. FIGURE 5 outlines the decision tree for sequencing evaluation and management of simple and complex cases. Matching the complexity of a patient with the complexity of the management strategy is the key to success. Once you develop the complete problem list, including contributing factors, it can provide criteria to distinguish simple and complex patients. Complexity of the patient increases with factors such as:
■ Presence of multiple comorbid conditions.
■ Persistent pain lasting longer than six months.
■ Significant emotional problems (depression, anxiety).
■ Frequent use of health care services or medication.
■ Daily oral parafunctional habits. ■ Significant lifestyle disturbances.
In addition, some complex patients warrant deferral of treatment until more complex problems are addressed. The criteria for not treating until these problems are resolved include factors such as:
■ Patient has primary chemical dependency.
■ Patient has primary psychiatric disorder.
■ Patient is involved in signs cant litigation.
■ Patient is overwhelmed with other concerns.
■ Patient is not motivated.
Once complexity is determined, the appropriate level of care that matches the complexity of the patient needs to be implemented (FIGURE 3). For example, a patient with acute self-limiting conditions can be managed with self-care strategy training from a health educator. TMD patients with multilevel problems require a second-order change that uses multimodal treatments as implemented by a single clinician. This integrative care strategy can include multiple treatments, such as splint, exercises, oral habit instruction, medication and palliative self care, to achieve second-order change with improvement over two to four months.
Use of a Health Care Team. Complex patients who have major life issues require a third-order change implemented by
an interdisciplinary team to achieve success. This transformative care strategy involves the team of clinicians, such as
a dentist, physician, health psychologist and physical therapist, working together with the patient to achieve success.66-68 Different specialists can address different aspects of the problem in order to enhance the overall potential for success. Teams can be interdisciplinary (one setting) or multidisciplinary (multiple settings). A team approach helps in understanding and managing the whole patient, allows multiple aspects of the problem to be treated simultaneously, improves patient compliance and outcome, saves time and is more economical and more enjoyable because the team works together.
To address every aspect of the problem, treatments may include cognitive-behavioral therapy, counseling, mindfulness meditation, physical medicine treatments, medications, splints, exercises with physical therapy, occlusal therapy and surgery. A consistent philosophy and message to the patient is needed, including the importance of self care, self responsibility and education using concepts of HST. Success depends on communication, integration among clinicians and proper patient selection. With complex patients, improvement, but rarely resolution, is typically achieved in six months. Interestingly, the economics of this model are quite favorable for each of the stakeholders, including the patient, the health care provider and the health plan. The patients receive more comprehensive effective care that is convenient if it is interdisciplinary in one setting. This not only has a higher potential to achieve success but also reduces the need for doctor shopping and single sequential trial-and-error treatments. Thus, the health plan’s long- term costs are reduced compared with a patient whose treatment continues to fail and who bounces from one doctor and intervention to another. Finally, the clinicians within a team practice benefit economically because more of them are providing care and generating income to cover the overhead of the practice. It’s a rare win-win-win scenario.
Principles of Management
Successful management of TMD is focused on treating the diagnosis and reducing the contributing factors in order to achieve the goals of:
■ Reducing or eliminating pain.
■ Restoring normal jaw function.
■ Restoring normal lifestyle functioning.
■ Reducing the need for future health care.
Once complexity is determined, the management options for TMD in general are consistent with treatment of musculoskeletal disorders in other parts of the body. The treatments involve interventions that have been documented with randomized controlled trials and are within the scope of dental practice to deliver or recommend.21-39 They include both reversible and irreversible treatments. Reversible treatments designed to encourage healing in the muscle and joints include self care, behavioral therapy, splints, medications and physical medicine. Irreversible treatments include joint surgery and permanent occlusal treatments. To determine whether the problem is self-limiting, self care should be initiated first. If the problem does not resolve within a few weeks and there is evidence of progression and/or persistence, treatment can proceed if pain and/or locking is severe enough to affect functioning or quality of life and the patient desires treatment. Each type of treatment is discussed briefly.
Reversible Treatments
Self Care. A key determinant of successful management of any musculoskeletal disorder involves educating the patient about the disorder and the necessity of compliance with the self-care aspects of management, including exercise, habit change and proper use of the jaw (TABLE 2).30,31 Information about self care should be provided to all patients and in some cases is the only strategy needed.
Behavioral Therapy. Approaches to changing maladaptive habits and behaviors should be addressed and presented as an integral part of the overall treatment program for all patients with TMD and poor oral habits.32,33 Behavior modi cation strategies are the most common techniques used to change habits. Although many simple habits will change when the patient is made aware of them, changing persistent habits requires a structured program facilitated by a clinician trained in behavioral strategies. Habit change using a habit reversal technique can be accomplished when the patient becomes more aware of the habit, learns how to correct it (i.e., what to do with the teeth and tongue) and knows why it is important to correct it.
When this knowledge is combined with a commitment to conscientious monitoring, most habits will change. Progress in changing habits should be addressed at all appointments. In some cases, patients may have significant psychosocial problems that accompany a TMD and may bene t from medication or counseling by a mental health professional. Prior to initiating treatment, a decision should be made as to whether the psychological distress is the primary problem. If this is the case, treatment of the psychological problem is best accomplished first and as an issue separate and apart from the TMD. Intraoral Splints. Splint therapy can be effective alone or in combination with other treatments for each stage of temporomandibular joint (TMJ) internal derangements and myofascial pain.22 Although there are many useful types of splints, four are commonly used for TMD: the full-arch stabilization splint, the anterior repositioning splint, the anterior bite plane and the posterior bilateral partial coverage splint. Complications that can occur with the use of any splint include caries, gingival inflammation, mouth odors, speech difficulties and/or psychological dependence on the splint.
The most serious complication is major irreversible changes in the occlusal scheme (open bites) that occur because of long- term use of partial coverage splints such as the anterior bite plane and the posterior coverage splint. Splints should not be designed to move teeth orthodontically during treatment of a TMD.
Pharmacotherapy. The most commonly used medications for pain are classified
as nonnarcotic analgesics (nonsteroidal anti-in ammatories), narcotic analgesics, muscle relaxants, tranquilizers (ataractics), sedatives and antidepressants.37-39 Analgesics are used to allay pain, muscle relaxants for muscle tension and nocturnal activity, tranquilizers for anxiety, fear and enhancing sleep and antidepressants for pain, depression and enhancing sleep.
Opioid analgesics have their own problems because of the potential for abuse and should be used sparingly and only with patients who have intractable chronic pain, no psychiatric conditions and no history
of chemical abuse. If prescribed, clinicians need to follow speci c opioid prescribing standards such as use of pain contracts, urine toxicology testing, suspension of medications with violation and other guidelines found at fsmb.org/pdf/2004_ grpol_Controlled_Substances.pdf.
Despite the advantages of medications for pain disorders, problems can occur because of their misuse. For this
reason, an important goal of treatment for most patients is to eliminate the
need for medications long term. With chronic pain patients, termination
of current medications should take precedence over prescribing additional ones. Problems that can occur from use of medications include chemical dependency, behavioral reinforcement of continuing pain, inhibition of endogenous pain relief mechanisms, side effects and adverse effects from the use of polypharmaceuticals.
Physical Medicine. The use of physical medicine techniques follows the same orthopedic and physical therapy guidelines as the evaluation and treatment of any musculoskeletal condition.23 Many exercises and modalities are available to help reduce pain and tenderness and increase range
of motion. Exercises are recommended to stretch, strengthen and relax muscles, to increase joint range of motion, to enhance muscle strength or to develop normal arthrokinematics. They are prescribed
in order to achieve specific goals and
are changed or modified as the patient progresses. Once the patient has reached the goals of the treatment, a maintenance level of exercise is recommended to assure long- term resolution of the patient’s problems.
In some cases of structural joint problems, limited range of motion and inflammation, ultrasound, iontophoresis, phonophoresis, superficial heat, cryotherapy and massage have been found helpful. Electrotherapies such as electrogalvanic stimulation and transcutaneous electrical stimulation have also been shown to be useful. Muscle and joint injections may also be recommended. However, these modalities typically have short-term effects and need to be used with exercises to maintain the improvement. For this reason, they should be used only until there is no longer a change in objective signs and/or improvement in pain.
Irreversible Treatments
In most cases, TMD problems improve with self care in combination with reversible treatments that encourage the natural healing processes of the muscles and joints. Irreversible treatments involve risk and should be used only if specific criteria are met. This applies to both TMJ surgery and permanent dental stabilization.
Surgery. TMJ surgery has become an effective treatment for structural TMJ disorders.34-36 However, the complexity
of available techniques, the potential for complications, the frequency of behavioral and psychosocial contributing factors and the availability of nonsurgical approaches mandate that TMJ surgery be used only in selected cases that meet specific criteria. The decision to treat a patient surgically depends on the degree of pathology present within the joint, the success or failure of appropriate nonsurgical therapy and the extent of disability that the joint pathology creates. A discussion of individual techniques is beyond the scope of this paper and can be found in the current American Association of Oral and Maxillofacial Surgery (AAOMS) position paper on TMJ surgery. Surgical management may vary from the closed surgical procedure (arthroscopy) to an open surgical procedure (arthrotomy), depending on the degree of disk deformity and degenerative changes. Each of the following criteria, adapted from the AAOMS criteria, should be fulfilled before proceeding with TMJ surgery:
■ Documented TMJ internal derangement or other structural joint disorder with appropriate imaging.
■ Evidence suggesting that symptoms and objective findings are a result of disk derangement or other structural joint disorder.
■ Pain and/or dysfunction of such magnitude as to constitute a disability for the patient.
■ Prior unsuccessful treatment with a nonsurgical approach that includes a stabilization splint, physical therapy and behavioral therapy.
■ Prior management of bruxism, oral parafunctional habits and other medical or dental conditions or contributing factors that will affect surgical outcome.
■ Patient consent after a discussion
of potential complications, goals, success rate, timing, postoperative management and alternative approaches, including no treatment.
These conditions maximize the potential for a successful outcome but cannot guarantee it. Patients with factors such as bromyalgia, depression or resistant nocturnal bruxism present with a complexity that has a poor prognosis. In addition, a full knowledge of complications and the reasons for surgical failure can help clinicians make this decision. Once this information is available, a realistic discussion of the prognosis, the patient’s expectations and any complicating factors can help
a patient make a correct decision about surgery. Postoperative physical and behavioral therapy should be integrated into the overall surgical management.
Permanent Dental Stabilization. Permanent dental treatment may be needed for some patients to provide
stable occlusal support and function
for the dental and temporomandibular structures.40 These treatments include occlusal adjustment, restorative dentistry, fixed or removable prosthodontics and orthodontics with or without orthognathic surgery. If needed because of poor
stability of the dentition, permanent treatment is recommended only after
pain has been reduced and normal
jaw function restored. The criteria for using secondary dental treatment to maintain comfort and function of the temporomandibular structures include:
■ The function and stability of the occlusion does not provide adequate orthopedic support. This may be due to missing teeth, skeletal malocclusion or gross interferences in dental function.
■ The lack of stable dental support is demonstrated to be directly related to aggravation or recurrence of the TMD after primary treatment of the disorder has been successfully completed.
Permanent dental treatment should proceed with the most conservative approach that will provide adequate function and stability of the occlusion. This ranges from occlusal adjustments to restorative dentistry to improve the dental occlusion and orthodontics to orthognathic surgery for changing the position of the teeth and skeletal relationships.
Conclusion
TMDs are common problems that can cause orofacial pain, jaw dysfunction and chronic head and neck pain, with
a collective estimated prevalence of at least 20 percent of the general population (TABLE 1).1-7 Because oral and craniofacial structures have close associations with functions of eating, communication, sight and hearing and form the basis for appearance, self-esteem and personal expression, they can deeply affect an individual’s psychological, behavioral and functional status.8 Thus, understanding TMD with a conceptual model that reflects a comprehensive and integrated problem list that is inclusive and flexible can better prepare clinicians to manage the full diversity of patients, from self limiting to simple to complex. A human systems approach and its related concepts can achieve this goal.
REFERENCES
1. Lipton JA, Ship JA, Larach-Robinson D. Estimated prevalence and distribution of reported orofacial pain in the United States. J Am Dent Assoc 1993. 124(10): p. 115-21.
2. Petti S. Pooled estimate of world leukoplakia prevalence: a systematic review. Oral Oncol 2003; 39: 770-780.
3. Lozada-Nur F, Miranda C. Oral Lichen Planus: Pathogenesis and Epidemiology. Semin Cutan Med Surg 1997; 16:290- 295.
4. Bailey D, Attanasio, R. Dentistry’s Role in the Management of Sleep Disorders: Recognition and Management. Dent Clin North America, edition on Sleep Disorders: Dentistry’s Role, WB Saunders Publishing Company, vol. 45(4): 619-630, 2001.
5. Taylor H, Curran NM. The Nuprin Pain Report. 1985, Louis Harris and Associates: New York.
6. Starch R. General Population Survey of Chronic Pain. Robert Starch Worldwide, 1999.
7. de Leeuw R (ed). Orofacial Pain — Guidelines for Assessment, Diagnosis and Management. 5th ed. Quintessence Publishing Company Inc.; 2013.
8. Engel GL. The Need for a New Medical Model: A Challenge for Biomedicine. Science new series, vol. 196, no. 4286. (April 8, 1977), pp. 129-136.
9. Suls J, Rothman A. Evolution of the Biopsychosocial Model: Prospects and Challenges for Health Psychology. Health Psychol vol. 23(2), Mar 2004, 119-125.
10. Borrell-Carrió F, Suchman AL, Epstein RM. The Biopsychosocial Model 25 Years Later: Principles, Practice and Scientific Inquiry. Ann Fam Med 2004 vol. 2(6): 576-582. 11. Bateson, G. (2000 reprint. First published 1972). Steps
to an Ecology of Mind: Collected Essays in Anthropology, Psychiatry, Evolution and Epistemology. University of Chicago Press. ISBN 0-226-03905-6. Retrieved March 19, 2013.
12. Bateson G. (1979) Mind and Nature: A Necessary Unity (Advances in Systems Theory, Complexity and the Human Sciences). Hampton Press. ISBN 1-57273-434-5.
13. Lorenz, Edward N. (1963) Deterministic Nonperiodic Flow. J Atmos Sci 20 (2): 130–141.
14. Kellert, Stephen H. (1993) In the Wake of Chaos: Unpredictable Order in Dynamical Systems. University of Chicago Press. p. 32. ISBN 0-226-42976-8.
15. Werndl C. (2009) What Are the New Implications of Chaos for Unpredictability? Brit J Philos Sci 60 (1): 195–220. doi:10.1093/bjps/axn053.
16. Keefe FJ. (2011) Behavioral medicine: a voyage to the future. Ann Behav Med 41, 141-151.
17. Feldman MD. (2012) Role of behavioral medicine in primary care. Curr Opin Psychiatr 25(2), 121-127.
18. Fredrickson BL. The value of positive emotions: The emerging science of positive psychology is coming to understand why it’s good to feel good. Am Sci vol. 91, no. 4, 2003, pp 330-335.
19. Lopez SJ, Snyder CR (ed.). The Oxford Handbook of Positive Psychology. Oxford University Press, 2011.
20. Fricton J. The Last Scroll: A Novel iUniverse (2013) www. thelastscroll.com and www.amazon.com/dp/1475975163/ ref=rdr_ext_tmb.
21. Fricton JR, Ouyang W, Nixdorf DR, Schiffman EL, Velly AM, Look JO. Critical appraisal of methods used in randomized controlled trials of treatments for temporomandibular disorders. J Orofac Pain 2010 Spring;24(2):139-51.
22. Fricton J, Look JO, Wright E, Alencar F, Chen H, Lang
M, Ouyang W, Velly AM. Systematic Review of Intraoral Orthopedic Appliance for Temporomandibular Disorders: 51 RCTs Reviewed. J Orofac Pain 24:237-54.2010.
23. Fricton J, Velly A, Ouyang W, Look J. Does exercise therapy improve headache? A systematic review with meta-analysis. Curr Pain Headache Rep 13(6):413-419, 2009.
24. Bussone G, Grazzi L, D’Amico D, Leone M, Andrasik F. Biofeedback-assisted relaxation training for young adolescents with tension-type headache: a controlled study. Cephalalgia 1998;18(7):463-7.
25. Loew TH, Sohn R, Martus P, Tritt K, Rechlin T. Functional relaxation as a somatopsychotherapeutic intervention:
a prospective controlled study. Altern Ther Health Med 2000;6(6):70-5.
26. Larsson B, Melin L, Doberl A. Recurrent tension headache in adolescents treated with self-help relaxation training and a muscle relaxant drug. Headache 1990;30(10):665-71.
27. Blanchard EB, Appelbaum KA, Radnitz CL, Michultka D, Morrill B, Kirsch C, et al. Placebo-controlled evaluation of abbreviated progressive muscle relaxation and of relaxation combined with cognitive therapy in the treatment of tension headache. J Consult Clin Psychol 1990;58(2):210-5.
28. Komiyama O, Kawara M, Arai M, Asano T, Kobayashi K. Posture correction as part of behavioural therapy in treatment of myofascial pain with limited opening. J Oral Rehabil 1999;26(5):428-35.
29. Turk DC, Rudy TE, Kubinski JA, Zaki HS, Greco CM. Dysfunctional patients with temporomandibular disorders: evaluating the efficacy of a tailored treatment protocol. J Consult Clin Psychol 1996;64(1):139-46.
30. Dworkin SF, Huggins KH, Wilson L, Mancl L, Turner J, Massoth D, et al. A randomized clinical trial using research diagnostic criteria for temporomandibular disorders-axis II to target clinic cases for a tailored self-care TMD treatment program. J Orofac Pain 2002;16(6):48-63.
31. Turner JA, Mancl L, Aaron LA. Brief cognitive-behavioral therapy for temporomandibular disorder pain: effects
on daily electronic outcome and process measures. Pain 2005;117(3):377-87.
32. Flor H, Birbaumer N. Comparison of the efficacy of electromyographic biofeedback, cognitive-behavioral therapy, and conservative medical interventions in the treatment
of chronic musculoskeletal pain. J Consult Clin Psychol 1993;61(4):653-8.
33. Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits: A meta-analysis. J Psychosom Res vol. 57, issue 1, pages 35-43, July 2004.
34. Miyamoto H, Sakashita H, Miyata M, Goss AN. Arthroscopic surgery of the temporomandibular joint: comparison of two successful techniques. Br J Oral Maxillofac Surg 1999;37(5):397-400.
35. Holmlund AB, Axelsson S, Gynther GW. A comparison
of discectomy and arthroscopic lysis and lavage for the treatment of chronic closed lock of the temporomandibular joint: a randomized outcome study. J Oral Maxillofac Surg 2001;59(9):972-7; discussion 77-8.
36. Schiffman EL, Look JO, Fricton JR, Hodges JS, Swift JQ, Decker KL, et al. A Randomized Clinical Trial Evaluating Four Treatment Strategies for Patients with Temporomandibular
Joint Disc Displacement without Reduction with Limited Mouth Opening. J Dent Res 2007 January; 86(1): 58–63.
37. Ta LE, Dionne RA. Treatment of painful temporomandibular joints with a cyclooxygenase-2 inhibitor: a randomized placebo-controlled comparison of celecoxib to naproxen. Pain 2004;111(1-2):13-21.
38. Mongini F, Bona G, Garnero M, Gioria A. Efficacy of meclofenamate sodium versus placebo in headache and craniofacial pain. Headache 1993;33(1):22-8.
39. Ekberg EC, Kopp S, Akerman S. Diclofenac sodium as an alternative treatment of temporomandibular joint pain. Acta Odontolo Scand 1996;54(3):154-9.
40. Fricton J. Current Evidence Providing Clarity in Management of Temporomandibular Disorders: A Systematic Review of Randomized Clinical Trials for Intraoral Appliances and Occlusal Therapies. J Evid Based Dent Pract March issue, vol. 6, issue 1, pp 48-52, 2006.
41. Velly AM, Gornitsky M, Philippe P. Contributing factors
to chronic myofascial pain: a case-control study. Pain 2003; 104(3): 491-9.
42. Fricton J, Nelson A. Monsein M. IMPATH: Microcomputer assessment of behavioral and psychosocial factors in craniomandibular disorders. J Craniomandibular Prac 5(4):372-381, 1987.
43. Schiffman E, Fricton J, Haley D. The relationship of occlusion, parafunctional habits and recent life events to mandibular dysfunction in a non-patient population. J Oral Rehabil 19:201-223, 1992.
44. Turner JA, Dworkin SF, Mancl L, Huggins KH, Truelove
EL. The roles of beliefs, catastrophizing and coping in the functioning of patients with temporomandibular disorders. Pain 2001; 92(1-2): 41-51.
45. Turner JA, Aaron LA. Pain-related catastrophizing: what is it? Clin J Pain 2001; 17(1): 65-71.
46. Gatchel RJ, Garofalo JP, Ellis E 3rd, Holt C. Major psychological disorders in acute and chronic TMD: an initial examination. J Am Dent Assoc 1996; 127(9): 1365-70, 72, 74.
47. Gatchel RJ, Peng YB, Peters ML, Fuchs PN, Turk DC. The biopsychosocial approach to chronic pain: scientific advances and future directions. Psychol Bull 2007; 133(4): 581-624. 48. Garofalo JP, Gatchel RJ, Wesley AL, Ellis E 3rd. Predicting chronicity in acute temporomandibular joint disorders using the research diagnostic criteria. J Am Dent Assoc 1998; 129(4): 438-47.
49. John MT, Miglioretti DL, LeResche L, Von Korff M, Critchlow CW. Widespread pain as a risk factor for dysfunctional temporomandibular disorder pain. Pain 2003; 102(3): 257-63.
50. Litt MD, Shafer DM, Ibanez CR, Kreutzer DL, Tawfik- Yonkers Z. Momentary pain and coping in temporomandibular disorder pain: exploring mechanisms of cognitive behavioral treatment for chronic pain. Pain 2009; 145(1-2): 160-8.
51. Litt MD, Shafer D, Napolitano C. Momentary mood and coping processes in TMD pain. Health Psychol 2004; 23(4): 354-62.
52. Rammelsberg P, LeResche L, Dworkin S, Mancl L. Longitudinal outcome of temporomandibular disorders: a five-year epidemiologic study of muscle disorders defined by research diagnostic criteria for temporomandibular disorders. J Orofac Pain 2003; 17(1): 9-20.
53. Wright AR, Gatchel RJ, Wildenstein L, Riggs R, Buschang P, Ellis E 3rd. Biopsychosocial differences between high-risk and low-risk patients with acute TMD-related pain. J Am Dent Assoc 2004; 135(4): 474-83.
54. Fillingim RB, Maixner W, Kincaid S, Sigurdsson A, Harris MB. Pain sensitivity in patients with temporomandibular disorders: relationship to clinical and psychosocial factors. Clin J Pain 1996; 12(4): 260-9.
55. Turner JA, Brister H, Huggins K, Mancl L, Aaron LA, Truelove EL. Catastrophizing is associated with clinical examination findings, activity interference, and health care use
among patients with temporomandibular disorders. J Orofac Pain 2005; 19(4): 291-300.
56. Velly AM, Look JO, Carlson C, Lenton PA, Kang
W, Holcroft CA, et al. The effect of catastrophizing and depression on chronic pain — a prospective cohort study of temporomandibular muscle and joint pain disorders. Pain 2011; 152(10): 2377-83.
57. Jensen MP, Romano JM, Turner JA, Good AB, Wald LH. Patient beliefs predict patient functioning: further support for a cognitive-behavioural model of chronic pain. Pain 1999; 81(1-2): 95-104.
58. Jensen MP, Turner JA, Romano JM. Changes in beliefs, catastrophizing and coping are associated with improvement in multidisciplinary pain treatment. J Consult Clin Psychol 2001; 69(4): 655-62.
59. Jensen MP, Turner JA, Romano JM. Correlates of improvement in multidisciplinary treatment of chronic pain. J Consult Clin Psychol 1994; 62(1): 172-9.
60. Jensen MP, Turner JA, Romano JM. Self-efficacy and outcome expectancies: relationship to chronic pain coping strategies and adjustment. Pain 1991; 44(3): 263-9.
61. Turner JA, Whitney C, Dworkin SF, Massoth D, Wilson L. Do changes in patient beliefs and coping strategies predict temporomandibular disorder treatment outcomes? Clin J Pain 1995; 11(3): 177-88.
62. Turner JA, Holtzman S, Mancl L. Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain 2007; 127(3): 276-86.
63. Jensen MP, Nielson WR, Turner JA, Romano JM, Hill ML. Changes in readiness to self-manage pain are associated
with improvement in multidisciplinary pain treatment and pain coping. Pain 2004; 111(1-2): 84-95.
64. Grzesiak RC. Psychologic considerations in temporomandibular dysfunction. A biopsychosocial view of symptom formation. Dent Clin North Am 1991; 35(1): 209-26. 65. Epker J, Gatchel RJ, Ellis E 3rd. A model for predicting chronic TMD: practical application in clinical settings. J Am Dent Assoc 1999; 130(10): 1470-5.
66. Gatchel RJ, Stowell AW, Wildenstein L, Riggs R, Ellis E
3rd. Efficacy of an early intervention for patients with acute temporomandibular disorder-related pain: a one-year outcome study. J Am Dent Assoc 2006; 137(3): 339-47.
67. Bell IR, Caspi O, Schwartz GER, Grant KL, Gaudet TW, Rychener D, Maizes V, Weil A. Integrative Medicine and Systemic Outcomes Research. Issues in the Emergence of
a New Model for Primary Health Care. Arch Intern Med 2002;162(2):133-140.
68. Mann D. Moving Toward Integrative Care: Rationales, Models, and Steps for Conventional-Care Providers. J Evid Based Complementary Altern Med October 2004 vol. 9 no.
3 155-172.
69. Fricton J, Hathaway K, Bromaghim C. The interdisciplinary pain clinic: outcome and characteristics of a long
term outpatient evaluation and management system. J Craniomandib Disord, 1(2):115-122, 1987.
THE AUTHOR, James Fricton, DDS, MS, can be reached at frict001@umn.edu.
James Fricton, DDS, MS, has devoted his career to patient care and research in temporomandibular and orofacial pain disorders. He is a senior researcher at the HealthPartners Institute for Education and Research and treats patients at the Minnesota Head and Neck Pain Clinic in Minneapolis. He is professor emeritus in the Department of Diagnostic and Surgical Sciences in the School of Dentistry at the University of Minnesota. Dr. Fricton has published and lectured extensively, is the author of TMJ and Craniofacial Pain: Diagnosis and Management, Myofacial Pain and Fibromyalgia and Advances in Orofacial Pain and TMJ Disorders and is serving as president of the International Myopain Society.
Conflict of Interest Disclosure: None reported.
Republished from CDA JOURNAL, VOL 4 2 , Nº 8 AUGUST 2014